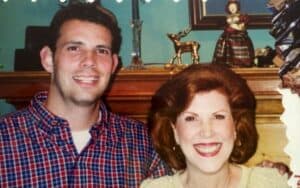
I don’t talk as much about my husband Jason’s caregiving journey, but he certainly had one. In our “spiral year” of 2014, he was almost four years into his primary caregiving role for his mom, who had stage 4 lung cancer.
The Backstory
Jason’s parents were still married when we started dating in high school. I was Jason’s date at his parent’s 25th wedding anniversary party. Jason is the youngest of two boys. His brother is almost five years older and lives in Arizona with his family. Jason was in college when his parents got divorced. At the time, both of Jason’s parents lived near us in metro Atlanta.
Sadly, Jason’s mom, Carol, was diagnosed with lung cancer in 2010.
Carol worked full-time in retail until her cancer progressed to a point where she could no longer do so. She didn’t own a house and no longer received alimony from her divorce. She drove a well-used car and lived in an affordable senior living apartment managed by the National Affordable Housing Management Association (i.e., subsidized housing for low-income seniors).
Carol’s savings was next to nil. When she needed extra funds, we were her first place to request financial help.
Carol lived alone and needed Jason’s constant attention. Jason and I were sandwich generation caregivers. On top of caring for our aging parents, we were raising our two adolescents and working full-time.
Some of the caregiving responsibilities Jason had in caring for his mom were:
- Medication management
- Grocery and supply shopping
- Securing meal delivery options
- Transportation
- Advocating for her well being
How Medicaid Can Help Families
It can be confusing to learn the differences between our two US government health assistance programs – Medicaid and Medicare. Medicare is generally available to every American age 65 and older. One harsh reality that new family caregivers come to learn is that Medicare does not pay for long-term care services.
Medicaid is America’s primary payer for long-term and eldercare services. Medicaid is a need-based program. According to the American Health Care Association, Medicaid covers more than 60 percent of all nursing home resident care.
Some of the programs Medicaid can offer assistance with include:
- Skilled nursing home
- Assisted Living or Independent Living Community
- Home care or home health aid
- Institutional care
- Substance use disorder services
The Medicaid application process is arduous because families are responsible for supplying financial and “clinically eligible” proof of a Medicaid need. And the requirements vary from state to state. Medicaid denies applications that are filled out incomplete or incorrectly.
Carol Needed Financial and Hands-On Help Managing Her Long-Term Care
At the time my husband initially requested Medicaid for his mom, Carol’s only source of income was her $870 a month Social Security check. After weeks of waiting for a reply, Medicaid rejected her application because she made ‘too much money.’ Through Carol’s multi-year cancer journey, my husband reapplied five times. Every request was declined.
To say my husband and I were frustrated by this application process and denial was an understatement. We were stunned that she was denied six times! We were disappointed that we had no options for her long-term care. We kept asking ourselves, “If Carol doesn’t qualify for Medicaid, then who does?!”
During this time, Jason and I paid out of pocket for professional caregivers to assist us with his mom’s care.
, personal care, counseling, volunteer respite, and companionship.
We Would Have Used This Service!
Thankfully, Ben Mandelbaum, a family caregiver and businessman working in the long-term care industry, repeatedly witnessed this problem with his clients. He got frustrated too, and became an expert in learning the Medicaid application system. Learn more about Ben’s story in this Happy Healthy Caregiver podcast episode.
Ben is the CEO of NavigAid. NavigAid is a tool available to families that simplifies the Medicaid process so people can focus on the care of themselves and their loved ones.

NavigAid is a secure online Medicaid application product that assists families and caregivers using an organized, step-by-step online format. NavigAid would have reduced the stress, time, and energy we experienced with Carol’s multiple Medicaid applications.
Would Carol still have been denied? Possibly. However, we would have felt confident knowing we applied correctly and been able to contact a NavigAid representative to answer our questions.
NavigAid is available in New York, New Jersey, Pennsylvania, Connecticut, Rhode Island, and Massachusetts. You can take a short quiz to determine if NavigAid could work in your situation. NavigAid has plans to expand to more states in the next few years.
NavigAid is affordable at $99! Traditional Medicaid application processing companies charge between $7,000-$10,00! I’m grateful that NavigAid has offered the Happy Healthy Caregiver community a 10% discount using the code ‘caregiver’ during the online checkout process.
Cost aside, NavigAid is a valuable resource for family caregivers. We welcome extra helping hands. The Medicaid question always pops up at the worst time! We often try to navigate this confusing world of Medicaid during a stressful time in our lives. A time when all we crave is less to do and more quality hours with our loved ones.

